Introduction
Allogeneic stem cell transplantation (alloSCT) can cure patients with hematological malignancies by T-cell mediated alloreactivity against patient hematopoiesis, the graft-versus-leukemia (GvL) effect. GvL can coincide with graft-versus-host disease (GvHD) when donor T cells target non-hematopoietic tissues. Increase of donor chimerism in bone marrow (BM) or peripheral blood (PB) after alloSCT indicates GvL response. After T-cell depleted alloSCT, donor lymphocyte infusion (DLI) can restore GvL. Dose and timing of DLI influence the degree of alloreactivity. Low dose of unmodified DLI as low as 0.3x10 6 T cells/kg 3 months after alloSCT appeared not to cause GvHD. (Zouwen et al. Ann Hematol, 2023) We hypothesized that infusion of a higher dose of purified CD4+ donor T cells would not cause GvHD, while inducing GvL by selective targeting of the MHC class II positive hematopoietic cells.
Method
A randomized controlled phase 2 trial was conducted in patients with hematological malignancies after HLA-identical sibling alloSCT with alemtuzumab added to the graft. Patients without GvHD or relapse were randomized at 2.5 months for prophylactic DLI with 1.0x10 6/kg CD4+ T cells (CD4+ DLI) 3 months after alloSCT or conventional care without DLI (CC). Both groups were eligible for prophylactic unmodified DLI at 6 months. Cumulative incidence (CI) of GvHD requiring immunosuppressive treatment 3 months after randomization was the primary endpoint. Changes in the trajectory of chimerism in BM and subsets in PB (CD4+ T cells, CD8+ T cells, NK cells, B cells and monocytes) were compared by means of mixed effects beta regression as secondary endpoints.
Results
66 patients were included (table 1). CI of GvHD did not differ between groups (CD4+DLI: 6.1% vs CC: 9.1%, Gray's test p>0.9). Relapse was comparable (CD4+DLI: 15% vs CC: 12%), although heterogeneity of diseases prevented a formal comparison.
In the CD4+ DLI group, BM chimerism was full donor (FD, >95% donor) at baseline in 23/33 patients, while 10/33 had mixed chimerism (MC, ≤95%). In the CC group, 23/33 were FD and 10/33 MC. Some patients with MC at baseline converted to FD in both groups (CD4+ DLI: 1/10 vs CC: 1/10). Changes in BM chimerism did not differ between CD4+ DLI and CC (p = 0.9). Chimerism of B cells, NK cells and monocytes in PB resembled bone marrow chimerism with most patients being FD at baseline. Changes in chimerism did not differ between CD4+ DLI and CC (p = 1.0, 0.5 and 0.9 for B cells, NK cells and monocytes respectively).
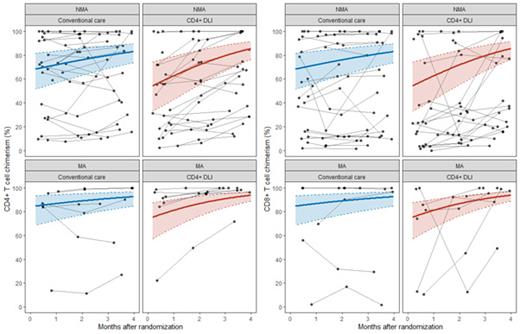
In the CD4+ DLI group, 25/30 evaluable patients were MC in the CD4+ T-cell subset in PB at baseline. 3 month after randomization 7/25 had converted to FD, 17/25 remained MC and 1/25 was unevaluable. Of the 17 patient who remained MC, CD4+ donor chimerism increased (absolute increase >5%) in 13, decreased (>5%) in 2 and was stable in 2. In the CC group, 26/32 were MC in CD4+ T cells at baseline, of which 6 converted to FD, 18 remained MC and 2 were unevaluable. Of the 18 patients remaining MC, CD4+ chimerism increased in 5, decreased in 9 and remained stable in 4. The CD4+ donor chimerism increased significantly after CD4+ DLI compared to CC (p = 0.01) (Figure 1).
In the CD4+ DLI group, 23/29 evaluable patients were MC in the CD8 subset at baseline. 7/23 converted to FD, 15/23 remained MC and 1 was unevaluable. Of these 15 MC patients at 3 months, 9 had increasing, 5 stable and 1 decreasing donor chimerism after 3 months. In CC, 22/31 were MC at baseline. 4/22 converted to FD at 3 months and 17/22 remained in MC. Of the 17 MC patients, 6 had increasing, 3 decreasing and 8 stable chimerism. The CD8+ donor chimerism increased significantly in the CD4+ DLI group compared to CC (p = 0.03).
Conclusion
CD4+ selected DLI at a dose of 1x10 6 CD4+/kg 3 months after HLA identical T-cell depleted alloSCT did not cause GvHD. Chimerism in BM leukocytes, B cells, NK cells or monocytes did not indicate GvL mediated by CD4+ DLI, possibly because most patients were already FD at baseline. CD4+ and CD8+ T-cell donor chimerism increased significantly after CD4+ DLI, suggesting a GVL-effect - earlier demonstrated in vitro for 4 selected patients. (Van Balen et al. Front Immunol, 2018) However, most patients did not convert to FD in the T-cell compartment, suggesting the GvL-effect of CD4+ DLI was limited. We considered this GvL-effect insufficient to prevent relapse and stress the importance of CD8+ donor T cells as main drivers of alloreactivity after DLI following HLA-identical alloSCT.
Disclosures
No relevant conflicts of interest to declare.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal